Stem Cell & Bone Marrow Transplants for Leukemia, Lymphoma, Myeloma
Stem cell and bone marrow transplants have revolutionized the treatment landscape for several types of blood cancers, including leukemia, lymphoma, and myeloma. These advanced therapies offer hope to patients who have exhausted other treatment options. In this comprehensive guide, we’ll delve into the intricacies of these transplants, their benefits, risks, and the procedure itself, providing a clear understanding of how they work and why they are a critical option for many cancer patients.
Introduction
Stem cell and bone marrow transplants are pivotal in the treatment of blood cancers such as leukemia, lymphoma, and myeloma. These procedures offer a chance for remission or even cure, particularly for patients who have not responded to traditional therapies. By understanding how these transplants work and their role in treating cancer, patients and their families can make informed decisions about their treatment options.
Understanding Blood Cancers
Understanding blood cancers involves recognizing various malignancies affecting the blood, bone marrow, and lymphatic system, such as leukemia, lymphoma, and multiple myeloma. Treating these cancers often requires a multifaceted approach, including medication like lenalidomide 5 mg. Lenalidomide is an oral drug that helps target and destroy cancerous cells by modulating the immune system and inhibiting the growth of abnormal cells.
What is Leukemia?
Leukemia is a cancer of the blood and bone marrow characterized by the overproduction of abnormal white blood cells. These cells crowd out healthy blood cells, leading to symptoms such as fatigue, frequent infections, and easy bruising. There are several types of leukemia, including acute and chronic forms, each with its own treatment challenges.
What is Lymphoma?
Lymphoma affects the lymphatic system, which is part of the body’s immune system. It involves cancers of the lymphocytes, a type of white blood cell. The two main types are Hodgkin lymphoma and non-Hodgkin lymphoma, each with distinct characteristics and treatment approaches.
What is Myeloma?
Myeloma, or multiple myeloma, is a cancer of the plasma cells, which are responsible for producing antibodies. It leads to the accumulation of abnormal plasma cells in the bone marrow, causing bone pain, anemia, and kidney problems. Treatment often involves a combination of medications and stem cell transplants.
The Basics of Stem Cell and Bone Marrow Transplants
Stem cell and bone marrow transplants are advanced treatments used to address various cancers and blood disorders. These procedures involve replacing damaged or diseased bone marrow with healthy stem cells to restore proper blood cell production and immune function. In addition to these transplants, medication such as lenalidomide 10mg plays a crucial role in managing cancer.
What are Stem Cells?
Stem cells are undifferentiated cells with the potential to develop into various cell types. They play a crucial role in replenishing damaged tissues and regenerating the blood and immune systems. In transplants, stem cells are used to replace damaged or destroyed bone marrow.
What is Bone Marrow?
Bone marrow is a spongy tissue inside bones where blood cells are produced. It contains stem cells that can transform into red blood cells, white blood cells, and platelets. Bone marrow transplants involve replacing diseased marrow with healthy marrow from a donor or from the patient themselves.
How Do Transplants Work?
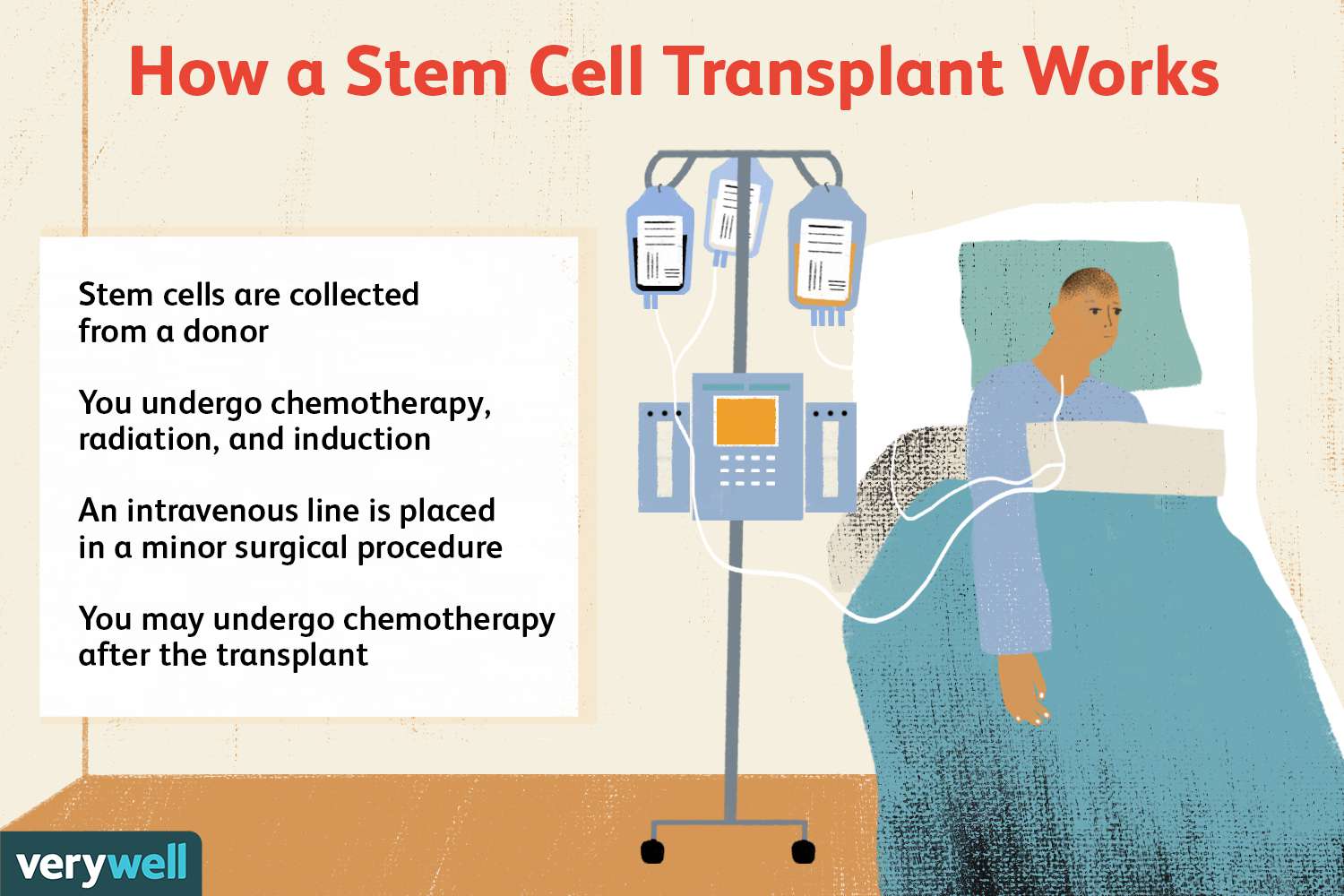
Transplants involve replacing diseased or damaged bone marrow with healthy stem cells. These cells can come from the patient (autologous transplant) or a donor (allogeneic transplant). The process includes a preparative regimen, the transplant itself, and a recovery period during which the new marrow establishes itself and begins to produce healthy blood cells.
Types of Stem Cell and Bone Marrow Transplants
Autologous Transplants
In an autologous transplant, stem cells are collected from the patient before treatment, then reintroduced after high-dose chemotherapy or radiation. This approach minimizes the risk of rejection and is often used for myeloma and lymphoma.
Allogeneic Transplants
Allogeneic transplants involve stem cells from a donor. This type of transplant is used when the patient’s own marrow is unable to produce healthy blood cells. Finding a compatible donor is crucial, and this type of transplant is used for leukemia and some lymphomas.
Syngeneic Transplants
A syngeneic transplant is a type of allogeneic transplant where the donor is an identical twin. Since the cells are genetically identical, the risk of rejection is significantly lower.
Indications for Stem Cell and Bone Marrow Transplants
When are Transplants Considered?
Transplants are typically considere when other treatments, such as chemotherapy or radiation, have ineffective. They may also recommended for patients with high-risk disease or those who relapse after initial treatment.
Eligibility Criteria for Patients
Eligibility for a transplant depends on various factors, including the type and stage of cancer, overall health, and the availability of a suitable donor. Each patient’s situation is assesse individually to determine the best course of action.
Preparing for a Stem Cell or Bone Marrow Transplant
Pre-Transplant Evaluation
Before the transplant, patients undergo thorough evaluations to assess their overall health and suitability for the procedure. This includes tests to check organ function, blood tests, and imaging studies.
Conditioning Regimen
The conditioning regimen involves high-dose chemotherapy or radiation to destroy cancer cells and suppress the immune system. This prepares the patient’s body to accept the new stem cells and reduces the risk of rejection.
Finding a Donor
For allogeneic transplants, finding a compatible donor is essential. This involves matching the patient’s human leukocyte antigens (HLAs) with those of potential donors. A perfect match reduces the risk of graft-versus-host disease (GVHD), where the transplanted cells attack the patient’s tissues.
The Transplant Procedure
Harvesting Stem Cells
Stem cells can harvested from the patient’s blood (peripheral blood stem cells), bone marrow, or umbilical cord blood. The method use depends on the type of transplant and the patient’s condition.
The Transplant Process
The actual transplant is similar to receiving a blood transfusion. The harvested stem cells are infuse into the patient’s bloodstream, where they travel to the bone marrow and begin to produce new blood cells.
Post-Transplant Care
Post-transplant care involves monitoring for complications, managing side effects, and supporting the patient’s recovery. This includes regular blood tests, medications to prevent infections, and supportive care to address any issues that arise.
Recovery and Side Effects
Short-Term Side Effects
Short-term side effects can include nausea, fatigue, mouth sores, and increased susceptibility to infections. These are typically manage with medications and supportive care.
Long-Term Side Effects
Long-term side effects may include fertility issues, organ damage, and an increased risk of secondary cancers. Regular follow-up appointments are essential to monitor and manage these effects.
Managing Complications
Complications such as graft-versus-host disease (GVHD) and infections are manage with medications and treatments tailored to the individual’s needs. Early detection and intervention are key to managing these issues effectively.
Success Rates and Prognosis
Factors Influencing Success Rates
Success rates depend on factors such as the type of cancer, the patient’s overall health, and the type of transplant. Advances in transplant techniques and supportive care have improved outcomes over the years.
Expected Outcomes for Different Cancers
The prognosis varies for different types of cancer. For example, stem cell transplants for myeloma have shown promising results, while outcomes for leukemia and lymphoma depend on factors like disease stage and response to prior treatments.