Anticoagulation Therapy: Indications, Risks, and Benefits
Introduction
Anticoagulation therapy is a cornerstone in the management and prevention of thromboembolic disorders, playing a critical role in reducing the risk of conditions like stroke, deep vein thrombosis (DVT), and pulmonary embolism (PE). Despite its life-saving potential, anticoagulation therapy is not without risks. Understanding the indications, potential complications, and benefits is essential for both healthcare providers and patients to ensure optimal outcomes.
Definition
In individuals who are at risk of thrombosis, anticoagulation therapy entails the use of drugs to stop blood clot formation. The way that these medications, such heparin or warfarin, function is by preventing blood clots, which lowers the risk of serious blood clotting inside blood vessels. For people with atrial fibrillation, this treatment is essential for treating diseases including deep vein thrombosis and pulmonary embolism as well as preventing stroke.
What is Anticoagulation Therapy?
Anticoagulation therapy involves the use of medications that inhibit the coagulation (clotting) process of blood. These medications, commonly referred to as blood thinners, do not actually thin the blood but rather prevent or reduce the formation of blood clots. Anticoagulants can be divided into two primary categories: injectable anticoagulants (such as heparin and low molecular weight heparin) and oral anticoagulants (such as warfarin and direct oral anticoagulants like apixaban and rivaroxaban).
Indications for Anticoagulation Therapy
The decision to initiate anticoagulation therapy is based on the presence of conditions that predispose an individual to the development of blood clots. The most common indications include:
1. Atrial Fibrillation (AFib)
Atrial fibrillation, an irregular and often rapid heart rate, increases the risk of stroke by promoting the formation of clots in the heart that can travel to the brain. Anticoagulation therapy is often recommended for patients with AFib to reduce the risk of stroke.
2. Venous Thromboembolism (VTE)
Venous thromboembolism includes both PE, in which a clot goes to the lungs, and DVT, in which a blood clot originates in the deep veins, commonly in the legs. Anticoagulants are the primary treatment for VTE to prevent the clot from growing and to reduce the risk of recurrence.
3. Mechanical Heart Valves
Patients with mechanical heart valves are at a high risk of thromboembolism because the artificial valve can cause blood to clot more easily. Lifelong anticoagulation therapy is typically required to prevent clots from forming on or around the valve.
4. Post-Surgical Prophylaxis
After major surgeries, particularly orthopedic procedures like hip or knee replacements, patients are at increased risk of developing blood clots. Anticoagulation therapy is often prescribed during the post-operative period to prevent thromboembolic events.
5. Stroke Prevention
In addition to atrial fibrillation, other conditions such as a history of transient ischemic attacks (TIAs) or previous strokes may warrant anticoagulation therapy to reduce the risk of future strokes.
Benefits of Anticoagulation Therapy
The primary benefit of anticoagulation therapy is its ability to significantly reduce the risk of thromboembolic events, which can be life-threatening. Key benefits include:
1. Stroke Prevention
Anticoagulation therapy can lower stroke risk in atrial fibrillation patients by as much as 70%. This is particularly important because strokes associated with AFib tend to be more severe and debilitating.
2. Reduction of Recurrence in VTE
In patients with a history of VTE, anticoagulation therapy reduces the risk of recurrence by approximately 80%. This is crucial in preventing the potentially fatal complication of pulmonary embolism.
3. Improved Outcomes in Heart Valve Replacement
For individuals with mechanical heart valves, anticoagulation therapy is essential for preventing clot formation on the valve, which can lead to valve malfunction or embolism.
4. Post-Surgical Clot Prevention
In the post-operative setting, anticoagulation therapy significantly reduces the risk of DVT and PE, allowing for safer recovery and reducing the need for further interventions.
Risks and Complications of Anticoagulation Therapy
Despite its benefits, anticoagulation therapy carries significant risks, primarily related to bleeding. These risks must be carefully weighed against the benefits in each patient.
1. Bleeding Complications
The most common and serious risk of anticoagulation therapy is bleeding. This can range from minor bruising or nosebleeds to life-threatening hemorrhages, such as gastrointestinal bleeding or intracranial hemorrhage. The risk of bleeding is influenced by factors such as the patient’s age, kidney function, and concurrent use of other medications that affect coagulation.
2. Monitoring and Drug Interactions
Patients on certain anticoagulants, like warfarin, require regular blood tests (INR monitoring) to ensure the drug is working effectively without increasing the risk of bleeding. Warfarin also has numerous drug and dietary interactions that can affect its efficacy, making management more complex.
3. Risk of Thrombosis
While rare, there is a paradoxical risk of thrombosis with some anticoagulants, particularly if they are not properly managed. For example, heparin-induced thrombocytopenia (HIT) is a serious condition where heparin triggers the formation of clots rather than preventing them.
4. Patient Compliance
Patient compliance has a major impact on the efficacy of anticoagulant therapy. Missing doses or discontinuing therapy without medical advice can significantly increase the risk of thromboembolic events. Conversely, taking too much of the medication can lead to serious bleeding.
5. Complications During Surgery
Patients on anticoagulation therapy who require surgery face additional risks, as the therapy increases the likelihood of surgical bleeding. Managing anticoagulation in the perioperative period requires careful planning, including the potential temporary discontinuation of the anticoagulant and bridging therapy with shorter-acting agents.
Balancing Risks and Benefits
The decision to initiate or continue anticoagulation therapy is a complex one that requires a personalized approach. Factors to consider include the patient’s risk of thromboembolism versus their risk of bleeding, the presence of other medical conditions, and lifestyle factors. For instance, older adults with atrial fibrillation may have a higher risk of bleeding, but the benefit of stroke prevention often outweighs this risk.
Risk Assessment Tools:
Clinicians often use risk assessment tools such as the CHA2DS2-VASc score for atrial fibrillation and the HAS-BLED score for bleeding risk to guide decision-making. These tools help in quantifying the risks and benefits, allowing for a more informed discussion with the patient.
Shared Decision-Making:
Shared decision-making is a key aspect of anticoagulation therapy. Patients should be fully informed about the risks, benefits, and potential side effects of the therapy. They should also understand the importance of adherence and regular monitoring, where applicable.
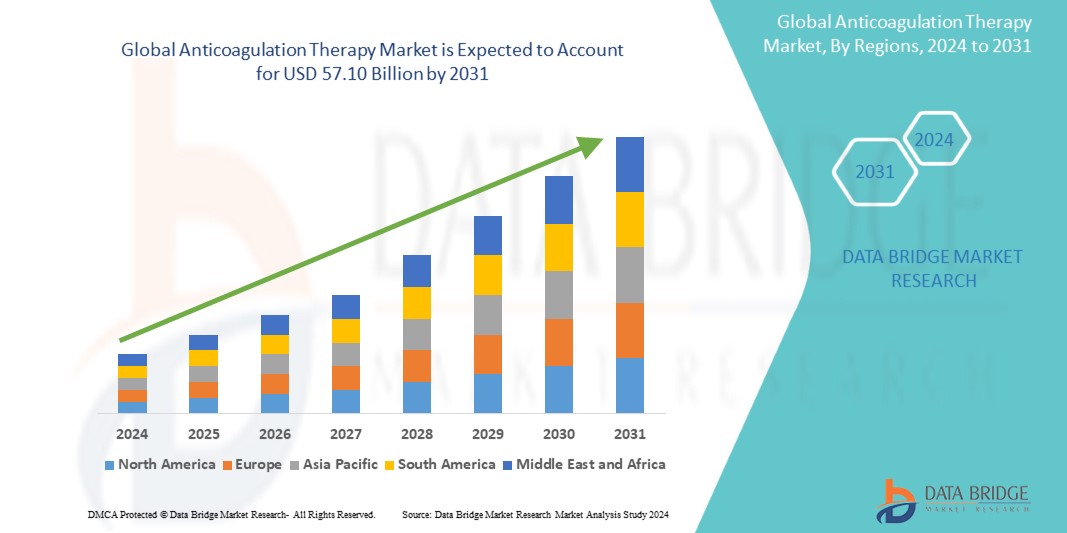
Growth Rate of Anticoagulation Therapy Market
The market for anticoagulant therapy was estimated to be worth USD 29.97 billion in 2023 and is expected to grow at a compound annual growth rate (CAGR) of 8.39% from 2024 to 2031, to reach USD 57.10 billion.
To explore more about Anticoagulation Therapy click here.
https://www.databridgemarketresearch.com/reports/global-anticoagulation-therapy-market
Conclusion
Anticoagulation therapy is a powerful tool in the prevention and treatment of thromboembolic diseases. While it offers significant benefits, particularly in reducing the risk of stroke and recurrent VTE, it is not without its challenges. The risks of bleeding and the need for careful management and monitoring underscore the importance of individualized care. Healthcare providers and patients must work together to ensure that anticoagulation therapy is used safely and effectively, maximizing its benefits while minimizing potential harms. Through careful consideration of indications, risk factors, and patient preferences, anticoagulation therapy can be a life-saving intervention for many individuals at risk of thromboembolic events.